Heparin, an anticoagulant discovered more than a century ago, is a popular blood thinner that prevents clotting. In mammals, it is made in small amounts by mast cells, a type of white blood cell. Heparin can be used to treat blood disorders and heart disease, but recently, scientists have begun exploring its potential therapeutic value for COVID-19.
In late March, a group of researchers based at Tongji Hospital in Wuhan, China, found that the relatively high mortality rate of severe COVID-19 was seemingly diminished in patients who had been treated with heparin.
As the ill recovered or passed away, the team found that overall, patients who had been administered heparin for its anticoagulant properties during their stay had a slightly better prognosis than those who had not.
“They found that the addition of heparin seemingly provided some sort of protective effect against viral infection,” says Nathan Lewis, a bioengineer at the Univ. of California, San Diego (UCSD). “We don’t know the exact mechanism, but there is preliminary evidence that shows the SARS coronavirus has some binding capabilities to heparin.”
If the virus is binding to heparin, it would have difficulty entering human cells, which would slow disease progression, says Lewis.
“You can imagine the virus attaching to these long chains of heparin and clumping up, unable to reach the cell. The answer is not yet clear, but I can say that our lab has some evidence of this mechanism.”
The connection between heparin and COVID-19 may be related to the higher risk of pulmonary embolism (i.e., lung clotting) in flu patients acutely ill with severe viral pneumonia and acute respiratory distress syndrome, a condition that some scientists have likened to severe COVID-19 infection. Severely ill flu patients have a 23-times higher risk for pulmonary embolism, according to a 2019 study.
Around the world, doctors and scientists have expressed growing concern about blood clotting in the lungs and its contribution to respiratory failure in severe COVID-19 patients. As an anticoagulant, heparin is an exciting prospect for possible treatment of the coronavirus.
Heparin is currently produced from harvested pig intestines, which contain an excess of mast cells. However, this is a messy and laborious process. Mast cells, which are the only mammalian cells that produce the anticoagulant, are not easily cultured at a scale large enough for mass production.
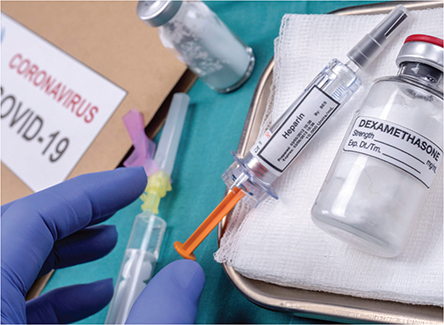
▲ Researchers at the Univ. of California, San Diego (UCSD) have developed a novel method for producing heparin, an anticoagulant. The blood thinner has potential therapeutic value for the treatment of COVID-19.
UCSD researchers are working on producing heparin through cell cultures, a practice that could make heparin more easily available to patients. In the past, it has been difficult to achieve recombinant production of heparin, i.e., production based on edited DNA in living cells.
Chinese hamster ovary (CHO) cells, the workhorse of the pharmaceutical industry, can easily be modified to produce therapeutic proteins such as insulin and growth hormones. But producing heparin in CHO or other mammalian cells has historically been difficult, as replicating the exact sulfate patterns present in the heparin molecule (C12H19NO20S3) is challenging. The enzymes critical to creating these patterns are not expressed adequately in CHO cells or in any cell lines.
The UCSD team has identified a transcription factor (ZNF263) that is a repressor of many (if not all) of the genes that code for these sulfation enzymes.
“This transcription factor is active in almost all cell types, and is basically repressing the cell’s ability to make heparin by limiting production of the enzymes,” says Lewis. “In mast cells, we found that ZNF263 is expressed at only low levels — so, the suppressor of heparin production is suppressed. Now, we have a gene that we can modify or eliminate to allow cells to produce the machinery needed to make heparin with the right sulfate patterns.”
The scientists discovered ZNF263 upon analyzing the genomic sequence surrounding the genes in the heparin synthesis pathway and finding a strong binding sequence for ZNF263. They hypothesized that this gene was essential to producing the enzymes and knocked out the gene, inducing a large increase in the production of metabolic pathways that contribute to heparin production.
In the future, the researchers hope to use genetic engineering to produce heparin in mammalian cells. They plan to modify the cells to produce sulfating enzymes at an adequate level for mass production of heparin. This technology could be useful for COVID-19 treatment, and potentially for other viruses.
“Recombinant heparin will emerge and replace much pig-produced heparin. It will be useful for future respiratory diseases or viral infections as a potential therapeutic,” says Lewis. In addition, with recent evidence that COVID-19 may persist in the future, he posits that the heparin technology may be useful. “But, I’m hoping that by the time our method is ready, we won’t be needing it for coronavirus anymore.”
Weiss, R. J., et al., “ZNF263 Is a Transcriptional Regulator of Heparin and Heparan Sulfate Biosynthesis,” Proceedings of the National Academy of Sciences, doi: 10.1073/pnas.1920880117 (Apr. 10, 2020).

Copyright Permissions
Would you like to reuse content from CEP Magazine? It’s easy to request permission to reuse content. Simply click here to connect instantly to licensing services, where you can choose from a list of options regarding how you would like to reuse the desired content and complete the transaction.

