Researchers at Duke Univ. have developed a miniature lung model grown in their laboratory that mimics the lungs’ air sacs, where COVID-19 infection typically takes place. This organoid (i.e., a simplified version of an organ) could allow engineers and scientists around the world to more closely understand the effects of corona virus on lung cells and the respiratory system.
SARS-CoV-2, the virus that causes COVID-19, gains entry through the nose or mouth and travels to the lungs, where it attacks stem cells called alveolar type-2 (AT2) cells. The lungs contain millions of AT2 cells, which are essential to the organ’s structural integrity and defense against invading pathogens.
Once AT2 cells are infected, they begin to die, leading to lung dysfunction. To rescue these cells, the immune system releases white blood cells in an attempt to overpower the virus. However, this immune response can damage the respiratory system — and while the extent of damage varies from patient to patient, in some cases, the respiratory damage can be severe and even fatal.
Much is still unknown about COVID-19 — for example, researchers are still investigating how it affects the heart, lungs, and nervous system, as well as how it affects certain demographics differently. Experimental models such as the Duke lung organoids can help fill some of these gaps.
“Experimental models are invaluable tools to understand the disease mechanism,” says Purushothama Rao Tata, a cell biologist at Duke. “One can use these models not only to understand how human cells behave in response to viral infection, but also to study the viral lifecycle. We can use this knowledge to develop better therapies for COVID-19 disease.”
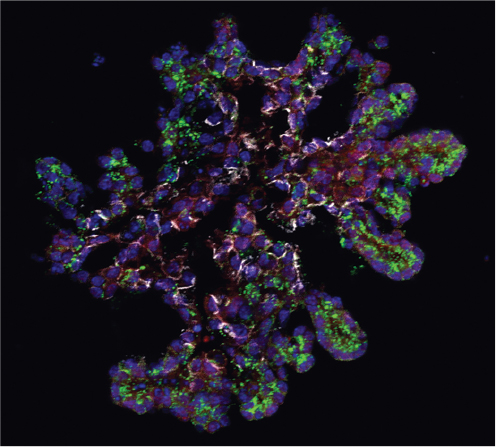
▲ Much is still unknown about SARS-CoV-2, the virus behind COVID-19. Scientists know how it enters the body, but know less about what happens once the virus is inside the heart, lungs, and nervous system. To obtain more information, researchers at Duke Univ. have developed an artificial lung model that mimics the lungs’ air sacs, where COVID-19 infection typically takes place. Image courtesy of Duke Univ.
While multiple models currently exist to study the process of COVID-19 infection, none of them contain a purified population of human AT2 cells, which are the key targets of SARS-CoV-2. The Duke team’s organoid model — which they call the mini lung — is derived entirely from AT2 stem cells.
To make the mini lungs, the researchers first obtained healthy human lung tissue. They sliced the tissue into small pieces and suspended it in media containing specialized enzymes that encourage robust cell growth.
Next, they isolated AT2 stem cells from the media and suspended them in a three-dimensional matrix supplemented with more growth media. Within 10–14 days, they were able to grow organoids made solely of AT2 stem cells. These stem cells assembled themselves into balloon-like structures that resembled human alveoli.
To test whether the AT2 cells function like real stem cells within human lungs, the researchers tested for expression of viral receptors ACE2 and TMPRSS2 — both of which are known to facilitate entrance of the coronavirus into the cell.
They found that the organoid strongly expressed these two receptors. Thus, the scientists had created a controlled environment where the artificial lung cells could mount an immune response to viral infection similar to the lungs of COVID-19 patients.
The next step for the team was to infect the mini lungs with SARS-CoV-2. One of their major goals was to better understand the impact of the virus on the AT2 cells, as well as how the cells respond to infection.
They confirmed that not only does SARS-CoV-2 block the replication of AT2 cells, but it also causes significant cell death. They also found that chemicals released by infected cells can negatively impact neighboring cells, causing the infection to spread.
“To our knowledge, this is the closest model to human lung AT2 stem cells,” says Tata. “This model will allow us to visualize the battle between the virus and human cells and give us a better understanding of the pathogenesis of the COVID-19 disease. We are currently using this new mini lung model to test the effects of drugs that are currently being used in clinical trials. In addition, we are using our platform to do large-scale genetic and pharmacological screens to identify new drugs that can potentially block SARS-CoV-2 entry and/or block its propagation in infected patients.”
Katusura, H., et al., “Human Lung Alveolospheres Provide Insights Into SARS-Cov-2 Mediated Interferon Responses and Pneumocyte Dysfunction,” Cell Stem Cell, doi: 10.1016/j.stem.2020.10.005 (Oct. 21, 2020).

Copyright Permissions
Would you like to reuse content from CEP Magazine? It’s easy to request permission to reuse content. Simply click here to connect instantly to licensing services, where you can choose from a list of options regarding how you would like to reuse the desired content and complete the transaction.

